Heron, M. & Anderson, R. N. Changes in the leading cause of death: Recent patterns in heart disease and cancer mortality. NCHS Data Brief. 254, 1–8 (2016).
Gjertsen, F., Bruzzone, S. & Griffiths, C. E. Burden of suicide presented as one of the leading causes of death: Uncover facts or misrepresent statistics?. J. Glob. Health https://doi.org/10.7189/jogh.09.010401 (2019).
Google Scholar
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Google Scholar
Leuven, E., Plug, E. & Ronning, M. Education and cancer risk. Labour Econ. 43, 106–121 (2016).
Google Scholar
Siegel, R. L. et al. An assessment of progress in cancer control. CA Cancer J. Clin. 68(5), 329–339 (2018).
Google Scholar
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68(6), 394–424 (2018).
Google Scholar
Bingham, S. & Riboli, E. Diet and cancer – The European prospective investigation into cancer and nutrition. Nat. Rev. Cancer 4(3), 206–215 (2004).
Google Scholar
Wilson, L., Bhatnagar, P. & Townsend, N. Comparing trends in mortality from cardiovascular disease and cancer in the United Kingdom, 1983–2013: Joinpoint regression analysis. Popul. Health Metr. https://doi.org/10.1186/s12963-017-0141-5 (2017).
Google Scholar
Williams, D. R., Priest, N. & Anderson, N. B. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychol. 35(4), 407–411 (2016).
Google Scholar
Shohaimi, S. et al. Residential area deprivation predicts fruit and vegetable consumption independently of individual educational level and occupational social class: A cross sectional population study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk). J. Epidemiol. Commun. H 58(8), 686–691 (2004).
Google Scholar
Teng, A. M., Atkinson, J., Disney, G., Wilson, N. & Blakely, T. Changing socioeconomic inequalities in cancer incidence and mortality: Cohort study with 54 million person-years follow-up 1981–2011. Int. J. Cancer 140(6), 1306–1316 (2017).
Google Scholar
Mirowsky, J. & Ross, C. E. Education, Social Status, and Health 1st edn. (Routledge, 2003).
Boylan, S. et al. Socio-economic circumstances and food habits in Eastern, Central and Western European populations. Public Health Nutr. 14(4), 678–687 (2011).
Google Scholar
Adler, N. E. et al. Socioeconomic status and health. The challenge of the gradient. Am. Psychol. 49(1), 15–24 (1994).
Google Scholar
Warnakulasuriya, S. Significant oral cancer risk associated with low socioeconomic status. Evid. Based Dent. 10(1), 4–5 (2009).
Google Scholar
Geyer, S., Hemstrom, O., Peter, R. & Vagero, D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J. Epidemiol. Community Health 60(9), 804–10 (2006).
Google Scholar
Ovrum, A. Socioeconomic status and lifestyle choices: Evidence from latent class analysis. Health Econ. 20(8), 971–984 (2011).
Google Scholar
Nordahl, H. et al. Education and cause-specific mortality: The mediating role of differential exposure and vulnerability to behavioral risk factors. Epidemiology 25(3), 389–396 (2014).
Google Scholar
Gallo, V. et al. Social inequalities and mortality in Europe–results from a large multi-national cohort. PLoS One 7(7), e39013 (2012).
Google Scholar
Hastert, T. A., Ruterbusch, J. J., Beresford, S. A., Sheppard, L. & White, E. Contribution of health behaviors to the association between area-level socioeconomic status and cancer mortality. Soc. Sci. Med. 148, 52–58 (2016).
Google Scholar
Lund Nilsen, T. I., Johnsen, R. & Vatten, L. J. Socio-economic and lifestyle factors associated with the risk of prostate cancer. Br. J. Cancer 82(7), 1358–1363 (2000).
Google Scholar
Conway, D. I. et al. Socioeconomic inequalities and oral cancer risk: A systematic review and meta-analysis of case-control studies. Int. J. Cancer 122(12), 2811–2819 (2008).
Google Scholar
Jepsen, P., Johnsen, S. P., Gillman, M. W. & Sorensen, H. T. Interpretation of observational studies. Heart 90(8), 956–960 (2004).
Google Scholar
Hernan, M. A. The hazards of hazard ratios. Epidemiology 21(1), 13–15 (2010).
Google Scholar
Schuit, A. J., van Loon, A. J., Tijhuis, M. & Ocke, M. Clustering of lifestyle risk factors in a general adult population. Prev. Med. 35(3), 219–224 (2002).
Google Scholar
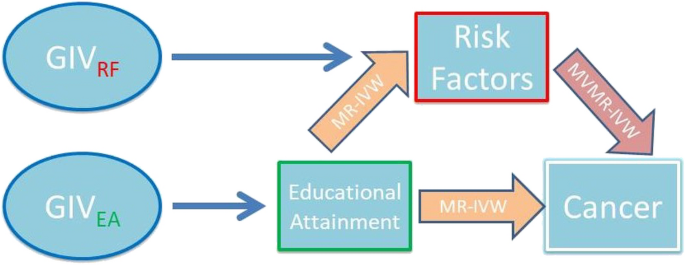
Smith, G. D. & Ebrahim, S. “Mendelian randomization”: Can genetic epidemiology contribute to understanding environmental determinants of disease?. Int. J. Epidemiol. 32(1), 1–22 (2003).
Google Scholar
Blakely, T., McKenzie, S. & Carter, K. Misclassification of the mediator matters when estimating indirect effects. J. Epidemiol. Community Health 67(5), 458–466 (2013).
Google Scholar
Davies, N. M., Holmes, M. V. & Davey, S. G. Reading Mendelian randomization studies: A guide, glossary, and checklist for clinicians. BMJ 362, k601 (2018).
Google Scholar
Thanassoulis, G. & O’Donnell, C. J. Mendelian Randomization nature’s randomized trial in the post-genome era. JAMA J. Am. Med. Assoc. 301(22), 2386–2388 (2009).
Google Scholar
Sudlow, C. et al. UK Biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PloS Med. 12(3), e1001779 (2015).
Google Scholar
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562(7726), 203 (2018).
Google Scholar
Okbay, A. et al. Polygenic prediction of educational attainment within and between families from genome-wide association analyses in 3 million individuals. Nat. Genet. 54(4), 437 (2022).
Google Scholar
Saunders, G. R. B. et al. Genetic diversity fuels gene discovery for tobacco and alcohol use. Nature 612(7941), 720 (2022).
Google Scholar
Liu, M. Z. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51(2), 237 (2019).
Google Scholar
Wootton, R. E. et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: A Mendelian randomization study. Psychol. Med. 50(14), 2435–2443 (2020).
Google Scholar
Leffondré, K., Abrahamowicz, M., Xiao, Y. L. & Siemiatycki, J. Modelling smoking history using a comprehensive smoking index: Application to lung cancer. Stat. Med. 25(24), 4132–4146 (2006).
Google Scholar
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in similar to 700,000 individuals of European ancestry. Hum. Mol. Genet. 27(20), 3641–3649 (2018).
Google Scholar
Elsworth B L, M, Alexander, T, Liu, Y, Matthews, P, Hallett, J, Bates, P, Palmer, T, Haberland, V, Smith, G D, Zheng, J., Haycock, P, Gaunt, T R, Hemani, G. The MRC IEU OpenGWAS data infrastructure. BioRxiv (2020).
Genomes Project C et al. An integrated map of genetic variation from 1092 human genomes. Nature 491(7422), 56–65 (2012).
Google Scholar
Palmer, T. M. et al. Using multiple genetic variants as instrumental variables for modifiable risk factors. Stat. Methods Med. Res. 21(3), 223–242 (2012).
Google Scholar
Burgess, S., Butterworth, A. & Thompson, S. G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 37(7), 658–665 (2013).
Google Scholar
Bowden, J., Smith, G. D. & Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44(2), 512–525 (2015).
Google Scholar
Bowden, J., Smith, G. D., Haycock, P. C. & Burgess, S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40(4), 304–314 (2016).
Google Scholar
Verbanck, M., Chen, C. Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50(5), 693 (2018).
Google Scholar
Mounier, N. & Kutalik, Z. Bias correction for inverse variance weighting Mendelian randomization. Genet. Epidemiol. 47(4), 314–331 (2023).
Google Scholar
Burgess, S., Dudbridge, F. & Thompson, S. G. Re: Multivariable Mendelian randomization: The use of pleiotropic genetic variants to estimate causal effects. Am. J. Epidemiol. 181(4), 290–291 (2015).
Google Scholar
Burgess, S., Daniel, R. M., Butterworth, A. S. & Thompson, S. G. Network Mendelian randomization: Using genetic variants as instrumental variables to investigate mediation in causal pathways. Int. J. Epidemiol. 44(2), 484–95 (2015).
Google Scholar
Sanderson, E. Multivariable Mendelian randomization and mediation. CSH Perspect. Med. https://doi.org/10.1101/cshperspect.a038984 (2021).
Google Scholar
RC T. R: A language and environment for statistical computing. R Foundation for Statistical Computing (2020).
Hemani, G. Z. J. et al. The MR-base platform supports systematic causal inference across the human phenome. elife https://doi.org/10.7554/eLife.34408 (2018).
Google Scholar
Gordon M L, T, Gordon, M M. R Package ‘forestplot’. Advanced Forest Plot Using ‘grid’ Graphics (2016).
Siegel, R., Ward, E., Brawley, O. & Jemal, A. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J. Clin. 61(4), 212–236 (2011).
Google Scholar
Gornick, M. E., Eggers, P. W. & Riley, G. F. Associations of race, education, and patterns of preventive service use with stage of cancer at time of diagnosis. Health Serv. Res. 39(5), 1403–1427 (2004).
Google Scholar
Mouw, T. et al. Education and risk of cancer in a large cohort of men and women in the United States. PLoS One 3(11), e3639 (2008).
Google Scholar
Cavelaars, A. E. et al. Educational differences in smoking: International comparison. BMJ 320(7242), 1102–1107 (2000).
Google Scholar
de Walque, D. Does education affect smoking behaviors? Evidence using the Vietnam draft as an instrument for college education. J. Health Econ. 26(5), 877–895 (2007).
Google Scholar
He, J. B., Chen, X. J., Fan, X. T., Cai, Z. H. & Huang, F. Is there a relationship between body mass index and academic achievement? A meta-analysis. Public Health 167, 111–124 (2019).
Google Scholar
De Irala-Estevez, J. et al. A systematic review of socio-economic differences in food habits in Europe: Consumption of fruit and vegetables. Eur. J. Clin. Nutr. 54(9), 706–714 (2000).
Google Scholar
Cooke, L. J. et al. Demographic, familial and trait predictors of fruit and vegetable consumption by pre-school children. Public Health Nutr. 7(2), 295–302 (2004).
Google Scholar
Rosoff, D. B. et al. Educational attainment impacts drinking behaviors and risk for alcohol dependence: Results from a two-sample Mendelian randomization study with ~780,000 participants. Mol. Psychiatr. 26(4), 1119–1132 (2021).
Google Scholar
O’Keeffe, L. M. et al. Smoking as a risk factor for lung cancer in women and men: A systematic review and meta-analysis. BMJ Open 8(10), e021611 (2018).
Google Scholar
Minami, Y. & Tateno, H. Associations between cigarette smoking and the risk of four leading cancers in Miyagi Prefecture, Japan: A multi-site case-control study. Cancer Sci. 94(6), 540–547 (2003).
Google Scholar
Pesch, B. et al. Cigarette smoking and lung cancer–relative risk estimates for the major histological types from a pooled analysis of case-control studies. Int. J. Cancer 131(5), 1210–1219 (2012).
Google Scholar
Larsson, S. C. et al. Smoking, alcohol consumption, and cancer: A mendelian randomization study in UK Biobank and international genetic consortia participants. PloS Med. 17(7), e1003178 (2020).
Google Scholar
Scherubl, H. Excess body weight and gastrointestinal cancer risk. Visc. Med. 37(4), 261–266 (2021).
Google Scholar
Vithayathil, M. et al. Body size and composition and risk of site-specific cancers in the UK Biobank and large international consortia: A mendelian randomization study. PloS Med. 18(7), e1003706 (2021).
Google Scholar
Menvielle, G. et al. The role of smoking and diet in explaining educational inequalities in lung cancer incidence. J. Natl. Cancer Inst. 101(5), 321–330 (2009).
Google Scholar
Wang, C., Yang, T., Guo, X. F. & Li, D. The associations of fruit and vegetable intake with lung cancer risk in participants with different smoking status: A meta-analysis of prospective cohort studies. Nutrients 11(8), 1791 (2019).
Google Scholar
Vieira, A. R. et al. Fruits, vegetables and lung cancer risk: A systematic review and meta-analysis. Ann. Oncol. 27(1), 81–96 (2016).
Google Scholar
Wang, J. et al. Citrus fruit intake and lung cancer risk: A meta-analysis of observational studies. Pharmacol. Res. 166, 105430 (2021).
Google Scholar
Fry, A. et al. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am. J. Epidemiol. 186(9), 1026–34 (2017).
Google Scholar
Park, J. H., Han, K., Hong, J. Y., Park, Y. S. & Park, J. O. Association between alcohol consumption and pancreatic cancer risk differs by glycaemic status: A nationwide cohort study. Eur. J. Cancer. 163, 119–27 (2022).
Google Scholar
Zhang, X. Y. et al. Alcohol consumption and risk of cardiovascular disease, cancer and mortality: a prospective cohort study. Nutr. J. 20(1), (2021).
Brion, M. J., Shakhbazov, K. & Visscher, P. M. Calculating statistical power in Mendelian randomization studies. Int. J. Epidemiol. 42(5), 1497–1501 (2013).
Google Scholar
Burgess, S. & Thompson, S. G. Bias in causal estimates from Mendelian randomization studies with weak instruments. Stat. Med. 30(11), 1312–1323 (2011).
Google Scholar
Rees, J. M. B., Wood, A. M. & Burgess, S. Extending the MR-Egger method for multivariable Mendelian randomization to correct for both measured and unmeasured pleiotropy. Stat. Med. 36(29), 4705–4718 (2017).
Google Scholar